A common problem faced by many diabetic patients is the ‘perceived’ or real inaccuracy of their glucometer. This happens when the glucose reading on the meter is widely different from what is expected – say a very high value after a usual walk that is known to reduce blood glucose or a very low value in a patient who’s not experiencing any symptoms.
When such aberrations occur the common tendency is to blame the glucometer. Some people claim that their glucometer has gone bonkers!However that may not be a good idea.
There are several standards that a blood glucose meter should satisfy before coming to the market. You can access these ISO standards here. Specifically 99% of readings must fall within zones A and B of the Consensus Error Grid for type 1 diabetes. Let me explain further.
What is an error grid ?
When a glucometer is validated for clinical or regulatory purposes, the values measured by the glucometer is compared with a reference method (method comparison study). A scatter plot is drawn and a grid is superimposed on the scatter graph.
For example, a pair (300 mg/dl, 550 mg/dl) represents a large numerical discrepancy, but is unlikely to result in an adverse clinical outcome since in either case the patient will probably receive insulin. On the other hand, a discrepancy of 70 vs. 110 could have serious clinical consequences since hypoglycemic therapy may be administered in the former case, possibly erroneously.
An error grid basically gives clinical context to the discrepancy in measurement between the two methods. Two major systems are in use : Clarke’s error grid and Parke’s(consensus) error grid.Both systems place paired reference/test values into one of five zones – “A”, “B”, “C”, “D” or “E” based on the expected clinical impact of the discrepency.
This is how Clarke’s and Parke’s Error grids look like
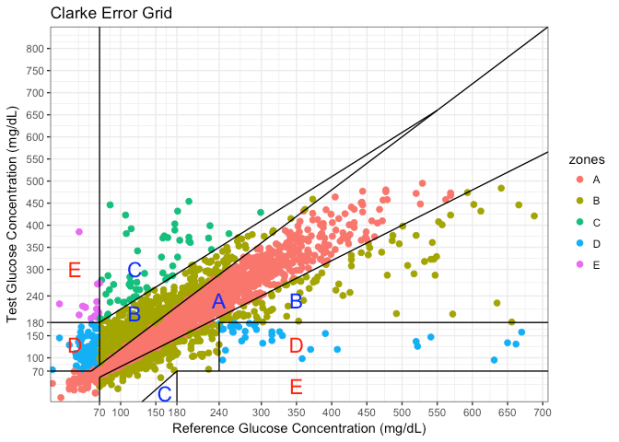
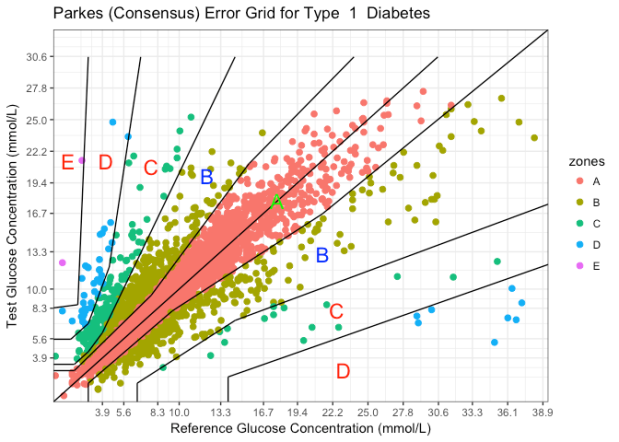
For regulatory clearance , 99 % of the values must fall within zone A or B. So glucometers from standard companies have a high bar to clear before they reach our hands.
In spite of all this, occasionally we get patients complaining of discrepant values. Let’s see what can be done if we get discrepant values. By going through a check list of questions, we can identify whether the reading is inaccurate and the source of inaccuracy.
- Wrong technique of pricking – usually minor
- Did you clean your fingers before pricking? This is common in children with type 1 diabetes/ the active type 2 diabetics who play/engage in outdoor activities. A finger that is covered with grime is unlikely to be accurate.Hence accurate cleaning is essential.
- Did you squeeze your finger hard? Squeezing fingers is not recommended because it leads to estimation of blood glucose in the interstitial fluid, not the capillary blood(the one we want). Choose a lancet , or prick with the appropriate size needle to ensure you get enough blood.
- Problem with glucose strip – uncommon
- Did you store the glucose strip properly? There is a reason glucostrips are packaged in black plastic containers. Exposure to excessive heat/moisture can lead to inaccuracy in glucose readings. Make sure that the glucose strip is stored correctly.
- Have you used the correct code ? Most modern gluco meters don’t require you to set the code manually.In case you are using a older version of glucometer, it is important to input the correct code. Otherwise wrong readings are possible.
- Has your strip expired? Glucose strips, like medicines, have expiry dates. It is important to make sure that the strip you are using is not an ancient one.
- Problem with glucometer
- Did you drop the glucometer recently? Glucometers are sensitive devices which should be handled with care. Dropping the glucometer from a height , (like any other electronic device) can result in glucometer malfunction.
- Water/heat or any other physical damage to the glucometer? Physical damage to the glucometer is easy to detect. You will have to replace the glucometer in this case.
If you have done all the steps correctly, and still have abnormal values, you need to don the Sherlock Holmes hat and see why it is happening.
Here are the steps to be followed
- Recheck again – this is the first step. If the second value is very similar to the first one, then perhaps error is not random. This of course, doesn’t mean that the value is correct. There could still be a systematic error (an example is a weighing machine that always shows you are 5 kg heavier:-)) . Systematic errors rarely happen in glucometers, but they are possible.
- If the repeat value is significantly different, (in spite of keeping all other conditions constant), then the technique is not the culprit. So the issue is with either the glucose strip or the glucometer.
- You have two options – check blood glucose with the nearby reliable lab or use a control solution. Control solutions contain a known amount of glucose and if the glucometer is working properly, it should be able to give the expected value. It is sort of like measuring a known 1 kg stone in an electronic weighing machine.If the machine shows abnormal reading, then something is wrong with the machine. However control solutions are not commonly used. Most pharmacies don’t event stock them and the glucometer doesn’t come with the control solution. The solution has to be purchased separately (can be got online) and once opened can be used for 3 months only. However they can be conveniently used at home.
Conclusions
- Standard glucometers go through stringent quality checks
- Whenever a discrepant glucose measurement is seen, think of the different levels where things can go wrong – patient, strip or glucometer
- When in doubt measure in a standard lab or use a control solution.
- As usual, proper patient education can avoid unnecessary confusion
Further reading
- Parkes, J. L., S. L. Slatin, S. Pardo, and B.H. Ginsberg. “A New Consensus Error Grid to Evaluate the Clinical Significance of Inaccuracies in the Measurement of Blood Glucose.” Diabetes Care 23, no. 8 (August 2000): 1143-48
- Pfutzner, Andreas, David C. Klonoff, Scott Pardo, and Joan L. Parkes. “Technical Aspects of the Parkes Error Grid.” Journal of Diabetes Science and Technology 7, no. 5 (September 2013): 1275-81

Difference between plasma and capillary glucose should also be remembered.pt can establish appropriate values by comparing capillary as well as plasma (lab value) done simultaneously.nice write up Dr Karthik. Congratulations
LikeLike
Yes indeed Dr Radha Rani. Thanks a lot for your encouragement 👍🙏
LikeLike
Thank you.
LikeLiked by 1 person
Glad you liked it 😊
LikeLike